Table of Contents
Reviewing Eligibility & Benefit Details
As patients are coming in for their appointments, you will want to start reviewing their benefits to prepare a treatment plan. To do this, simply navigate to your desired appointment date on the daily huddle page.
For completed checks, you will click on the patients name to start reviewing their benefits. From here you will see a few four tabs.
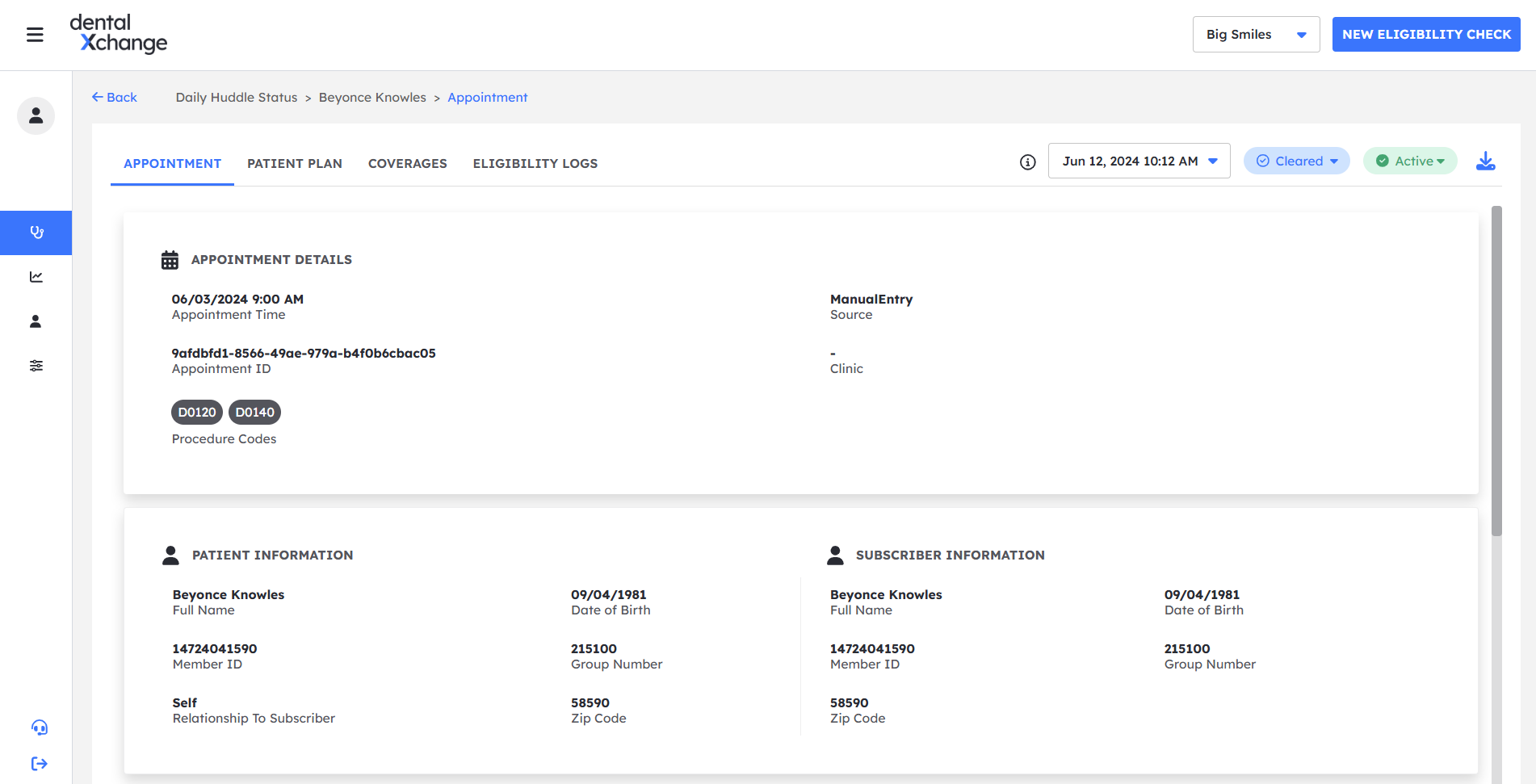
Appointment
The appointment tab is where you will find all the information pertaining to the patient you selected. This information is the same as what's available by clicking the "eye" icon on the daily huddle page. Listed from the top of the page is: Any "error" messages that might of come back from the check, Appointment Details, Patient/Subscriber information, Provider/Insurance details and Appointment Notes where you can add anything note worthy here for the appointment.
Patient Plan
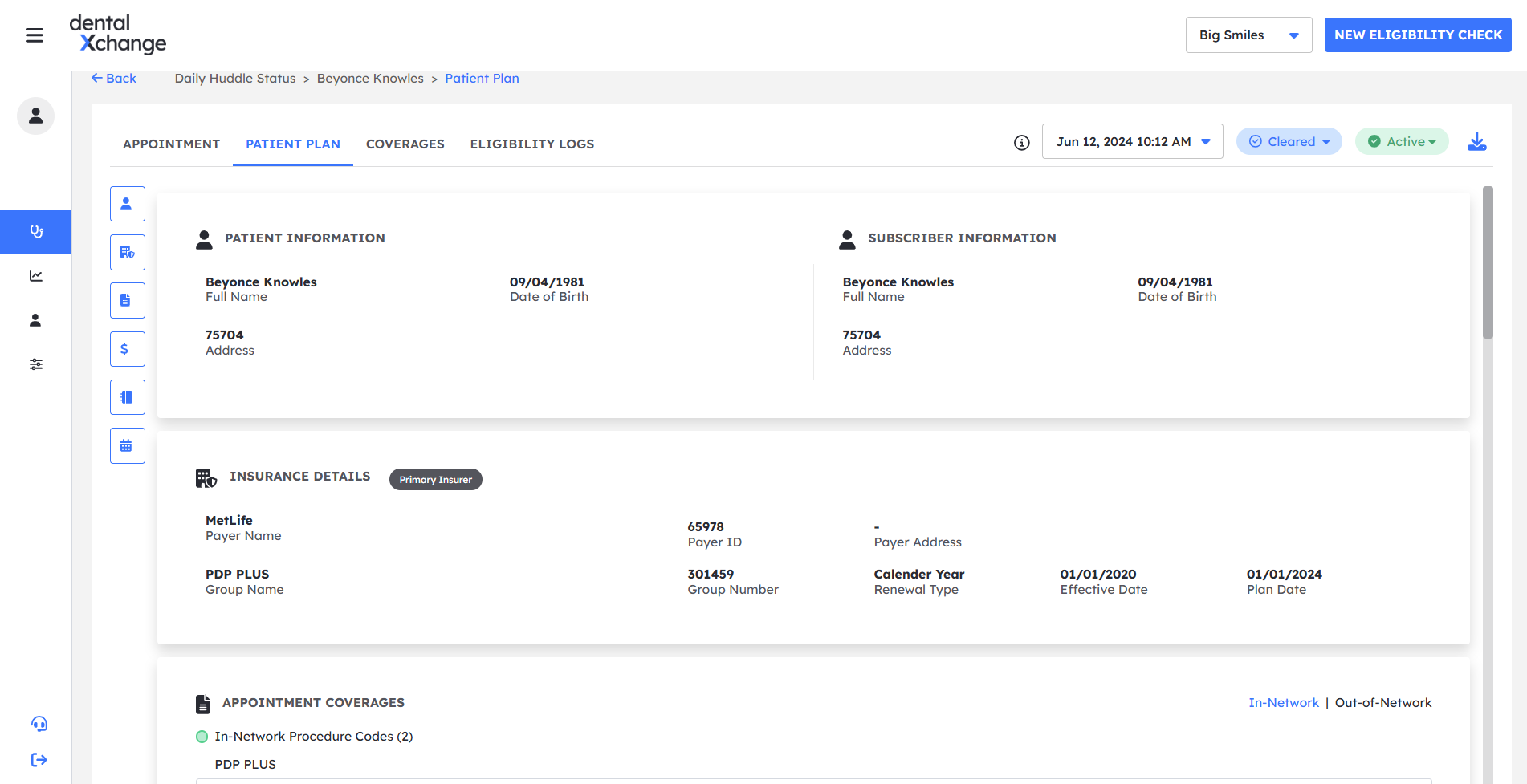
Under this tab, you will find the patient's plan information. It shows key details for the subscriber level plan details. One benefit of Eligibility AI is that our benefit details are down to the patient level so you will see maximum and deductible amounts used and remaining across all dental offices.
- Patient & Subscriber Information — this section gives you a glimpse of the patient and subscribers key demographics such as name, date of birth, and address.
- Insurance Details — this section is the first amount of data Eligibility AI receives from the payer. It includes important details such as the plan date, effective date, and renewal type. The plan date and renewal details are key to determining benefit limitations such as, 2 covered procedures per year, 1 per lifetime, etc.
- Appointment Coverages — this section includes the benefit details specific to this appointment. While the full benefit details are available in the Coverages tab, the Appointment Coverages is simply a filtered down view. You can switch between In-Network and Out-of-Network for the coverages by clicking each network.
- Plan Maximum — this section includes the service year and plan year maximums for the patient including both individual and family coverages (if applicable). Just like Appointment Coverages, you can easily switch between In-Network and Out-of-Network maximums. The maximums are displayed in an easy to read format with the remaining amount for the year inside the circle and the total used shown below the circle.
- Plan Deductible — similar to the Plan Maximum, this section shows any applicable plan level deductibles.Plan Maximums and Deductibles apply across all dental offices which have submitted claims for this patients insurance. If the patient received services from another office and the plan paid out the claim, the plan maximum generally will reflect that in the remaining and used amounts.
- Service History — the last section in the Patient Plan tab covers the service history as it's available from the payer. Just like plan maximums and deductibles, this includes all service history across all offices.
Coverages
The Coverages tab is the complete listing of benefits by procedure code and benefit class as available on the payers website. It will allow you to see all the various procedure codes, and how they are covered for the patient you have pulled up. By default, everything will be condensed, however each benefit class can be expanded to show more. You can also filter to a specific benefit class with the drop down towards the top of the tab, next to the "expand all" button. You can use the search bar to find a specific procedure code either by typing the CDT number or just simply the procedure name. You can also filter by in or out of network coverage and by the network name (if available).
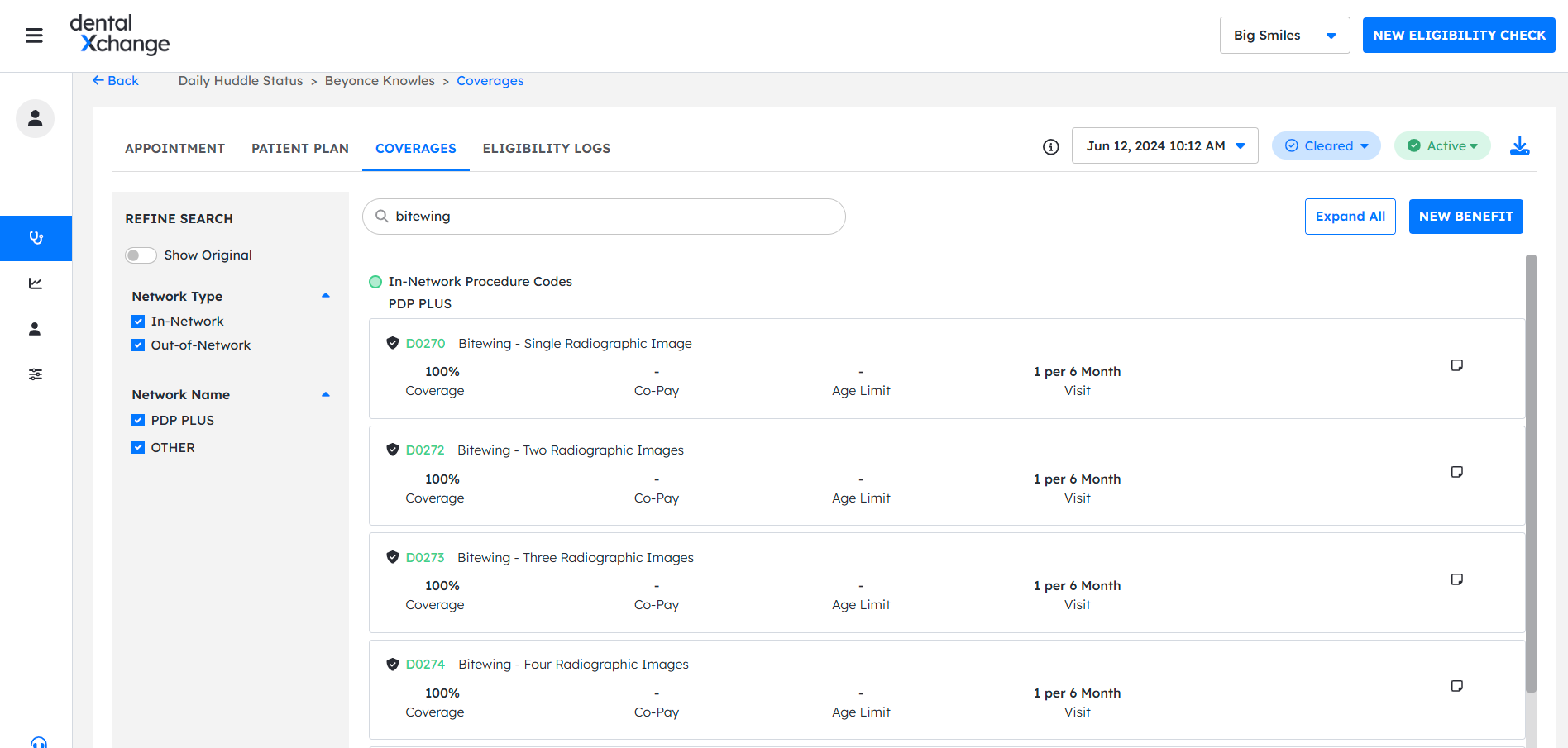
When viewing coverage rows, you will be able to view the last service date, co-insurance amount, procedure code level co-pays, age limits, and any frequency limitations.
Logs
Logs is where you can view previously run eligibility checks for the patient. It will list the date and time of the appointment as well as when the check was run, what procedure codes were listed on the appointment, the status of the check, the insurance status for the patient as of that check, and finally the "page" action button that will take you to the appointment for that day the check was run.
